Novel Use of a Self-Expandable Metal Stent with an Anti-Migration System for Palliative Drainage of a Pancreatic Cystic Neoplasm
DOI:
https://doi.org/10.6092/1590-8577/2802Keywords:
Endoscopy, Digestive System, Gastric Outlet Obstruction, Pancreatic Cyst, Pancreatic NeoplasmsAbstract
Context There is scanty data on endoscopic palliative management of pancreatic cystic lesions that cause gastric outlet obstruction (GOO). This is the first case report that illustrates the use of a covered self-expandable metal stent (CSEMS) with an anti-migration system in the management of a symptomatic neoplastic cystic pancreatic lesion. Case report A 92-year-old Chinese female presented with partial GOO for 3 months. Examination revealed a non-tender epigastric mass with moderate abdominal distension. Esophagogastroduodenoscopy (EGD) showed a significant bulge at the posterior wall of the gastric antrum and food residue in the stomach. A CT scan of the abdomen showed a large pancreatic tail cystic lesion. Endoscopic ultrasound (EUS) showed a clear, non-septated cystic lesion measuring 9.7x10 cm arising from the pancreatic tail. Analysis of the aspirate revealed the following: Amylase: 3,200 units/L, CEA: 411 ng/mL, CA 19-9 812 U/mL and no malignancy. A Niti-STM Biliary Stent (NAGITM) was used for a cystogastrostomy. This procedure was complicated by a self-limiting intra-abdominal leak, stent migration and bleeding from a splenic artery pseudoaneurysm which was arrested with coil embolization. She progressed well after that with significant symptom improvement and no further complications. Conclusion This is the first case of a CSEMS with an anti-migration system that was used for decompression of a pancreatic cystic neoplasm (PCN). Novel use of this stent is a viable option as palliative management of a PCN in those not fit for surgery but caution needs to be exercised as there can be significant complications.
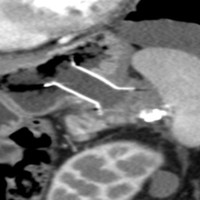
Image: CT abdomen showing stent in-situ.
Downloads
References
Yamamoto N, Isayama H, Kawakami H, Ito Y, Takahara N, Uchino R, et al. Preliminary report on a new, fully covered, metal stent designed for the treatment of pancreatic fluid collections. Gastrointest Endosc. 2013; 77: 809-814.[PMID: 23453183].
Itoi T, Nageshwar Reddy D, Yasuda I. New fully-covered self-expandable metal stent for endoscopic ultrasonography-guided intervention in infectious walled-off pancreatic necrosis (with video). J Hepatobiliary Pancreat Sci. 2013; 20: 403-406.[PMID: 22926337].
Tanaka M, Fernandez-del Castillo C, Adsay V, Jang JY, Kimura W, Levy P, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012; 12: 183-197.[PMID: 22687371].
Silva RG, Jr., Silverman WB, Gerke H. Palliative endoscopic ultrasound-guided drainage of a malignant pancreatic cyst causing gastric outlet obstruction. Pancreatology. 2006; 6: 472-476. [PMID: 16847385].
Oh HC, Seo DW, Lee TY, Lee SK, Kim MH. New treatment for cystic tumors of the pancreas: EUS-guided ethanol lavage with paclitaxel injection. Gastrointest Endosc 2008; 67: 636-642. [PMID: 18262182].
Varadarajulu S, Christein JD, Wilcox CM. Frequency of complications during EUS-guided drainage of pancreatic fluid collections in 148 consecutive patients. J Gastroenterol Hepatol. 2011; 26: 1504-1508.[PMID: 21575060].
Ahn JY, Seo DW, Eum J, Moon SH, Park do H, Lee SS, et al. Single-Step EUS-Guided Transmural Drainage of Pancreatic Pseudocysts: Analysis of Technical Feasibility, Efficacy, and Safety. Gut Liver. 2010; 4: 524-529.[PMID: 21253303].
Bergert H, Dobrowolski F, Caffier S, Bloomenthal A, Hinterseher I, Saeger HD. Prevalence and treatment of bleeding complications in chronic pancreatitis. Langenbecks Arch Surg. 2004; 389: 504-510. [PMID: 15173947].
Furukawa H, Fukushima N, Shimada K. Splenic artery aneurysm secondary to pancreatic carcinoma. Am J Gastroenterol. 2000; 95: 3659-3660. [PMID: 11151921].
Han YM, Lee JY, Choi IJ, Kim CG, Cho SJ, Lee JH, Kim HB, Choi JM. Endoscopic removal of a migrated coil after embolization of a splenic pseudoaneurysm: a case report. Clin Endosc. 2014; 47: 183-187. [PMID: 24765602].